(1) Sariali E, Mouttet A, Pasquier G, Durante E, Catone Y. Accuracy of reconstruction of the hip using computerised three-dimensional pre-operative planning and a cementless modular neck stem. J Bone Joint Surg Br. 2009 Mar;91(3):333-40.
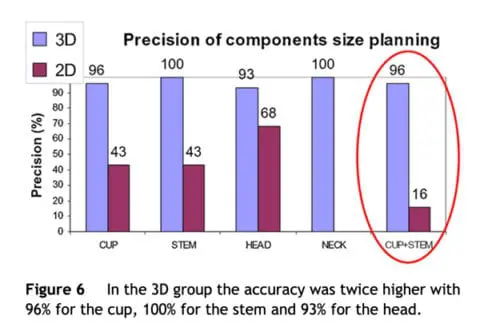
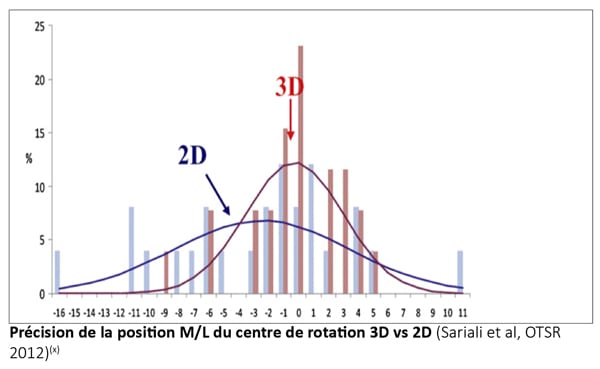
(2) Sariali E, Mauprivez R, Khiami F, Pascal-Mousselard H, Catonné Y. Accuracy of the preoperative planning for cementless total hip arthroplasty. A randomised comparison between three-dimensional computerised planning and conventional planning. Orthop Traumatol Surg Res. 2012 Apr;98(2):151-8.
(3) Hassani H, Cherix S, Ek ET, Rüdiger HA. Comparisons of preoperative three-dimensional planning and surgical reconstruction in primary cementless total hip arthroplasty. J Arthroplasty. 2014 Jun;29(6):1273-7.
(4) Sariali E, Boukhelifa N, Catonne Y, Pascal Mousselard H. Comparison of three-dimensional planning-assisted and conventional acetabular cup positioning in total hip arthroplasty: A randomized controlled trial. J Bone Joint Surg Am. 2016 Jan 20;98(2):108-16.
(5) Sariali E, Klouche S, Mouttet A, Pascal-Moussellard H. The effect of the femoral offset modification on gait after total hip arthroplasty. Acta Orthop. 2014 Apr;85(2):123-7.
(6) Sariali E, Klouche S, Mamoudy P. Ceramic-on-ceramic total hip arthroplasty: Is squeaking related to an inaccurate three-dimensional hip anatomy reconstruction? Orthop Traumatol Surg Res. 2014 Jun;100(4):437-40.
(7) Sariali E, Stewart T, Jin Z, Fischer J. In vitro investigation of friction under edge-loading conditions for ceramic-on-ceramic total hip prosthesis. J Orthop Res. 2010 Aug;28(8) :979-85.
(8) Patel A B, Wagle R R, Usrey M M, Thompson M T, Incarvo S J, Noble P C. Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty. 2010 Dec;25(8):1275-81.e1.
(9) Asayama I, Chamnongkich S, Simpson K J, Kinsey T L, Mahoney O M. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005 Jun;20(4):414-20.
(10) McGrory B J, Morrey B F, Cahalan T D, An K N, Cabanela M E. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995 Nov;77(6):865-9.
(11) Sakalkale D P, Sharkey P F, Eng K, Hozack W J, Rothman R H. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001 Jul;(388):125-34.
(12) Charles M N, Bourne R B, Davey J R, Greenwald A S, Morrey B F, Rorabeck C H. Soft-tissue balancing of the hip: the role of femoral offset restoration. J Bone Joint Surg Am. 2004;86:1078-1088.
(13) Flecher X, Ollivier M, Argenson JN. Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res. 2016 Feb;102(1 Suppl):S9-20.
(14) Pasquier G, Ducharne G, Sari Ali E, Giraud F, Mouttet A, Durante E. Total hip arthroplasty offset measurement: is CT scan the most accurate option? Orthop Traumatol Surg Res. 2010 Jun;96(4):367-75.
(15) Huppertz A, Radmer S, Asbach P, Juran R, Schwenke C, Diederichs G, Hamm B, Sparmann M. Computed tomography for preoperative planning in minimal-invasive total hip arthroplasty: radiation exposure and cost analysis. Eur J Radiol. 2011 Jun;78(3):406-13.