With more than 25,000 individualized-designed stems, and over 30 years’ clinical experience, the INDIVIDUAL HIP® stem is the benchmark in individualized hip replacement.
Clinical experience of the concept, and 25 years of published knowledge (1)
20-year survival for patients under 50 years of age (1)(2)

to replicate the proximal femur
Femoral morphology varies greatly from one person to another in the three dimensions of space. Research conducted by Husmann (3) and Sariali (4) has demonstrated these variations in the proximal femur and hip in 3D, even in cases often considered “normal”. In some rarer cases, the hip anatomy can be dysplastic and deviate greatly from the anatomical averages for which standard hip prostheses were designed.
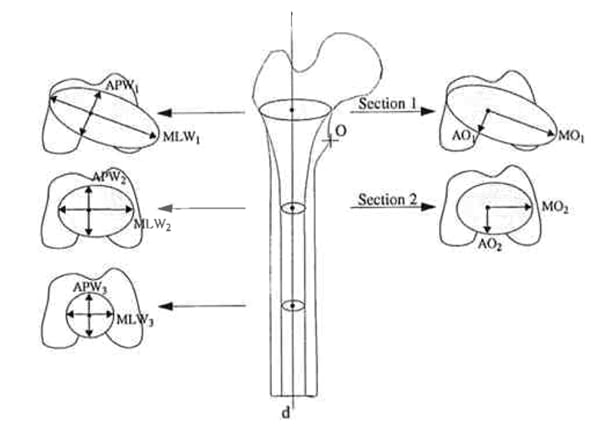
Each individual is different, so the INDIVIDUAL HIP® stem is designed to adapt perfectly to the shape of the medullary canal in all three dimensions, so no need for compromise:

Symbios’ engineers identify the preferred support zones between the bone and the prosthesis within the metaphyseal zone to:

A individualized compactor identical to the implant is delivered for each patient, to prepare the medullary canal before implanting the final stem.


for no-compromise hip reconstruction
Work undertaken by Krishnan (5) has shown that there is no correlation between medullary canal size and femoral offset. Standard implants often become limited because of their homothetic design when the femoral offset to be restored is not proportional to the size of the canal.
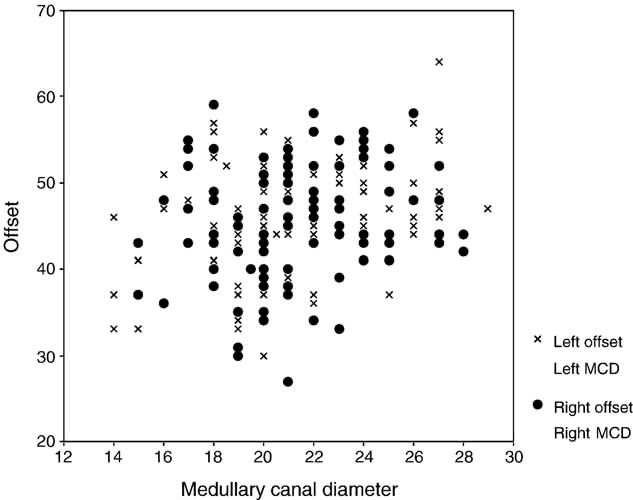
The individualized stem has a neck designed to reconstruct the joint by restoring the centre of rotation with no compromise based on the planned stem position.

The stem is designed to restore femoral anteversion in a personalised manner and to maximise anterior-posterior stability and joint function.


to accommodate surgical preferences
In addition to adapting to the patient, the individualized stem adapts to the standard practices of each surgeon, with a multitude of options and variants:


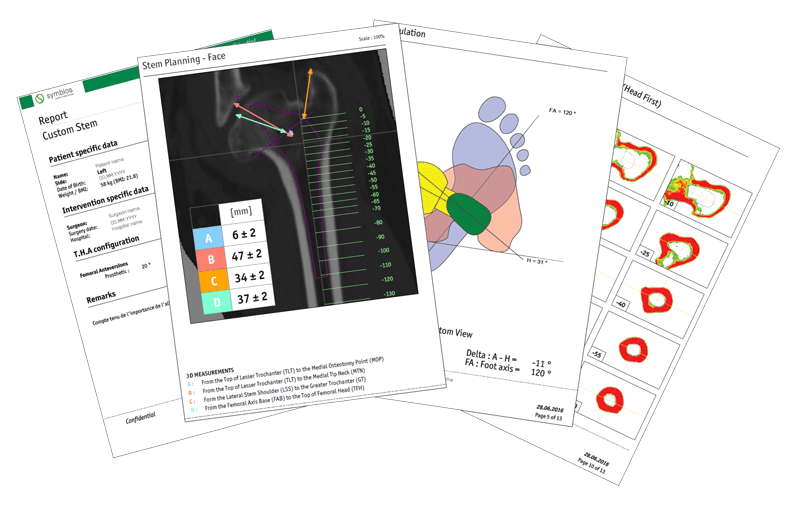
The INDIVIDUAL HIP® stem comes with the planning report, to guide the surgeon throughout the procedure.